Atsuhiko Yamamoto, DDS, PhD
Lecturer, The Japan Institute for Advanced Dental Studies (JIADS), Osaka and Tokyo, Japan;
President, Perio-Implant Hospital AUTIS, Osaka, Japan
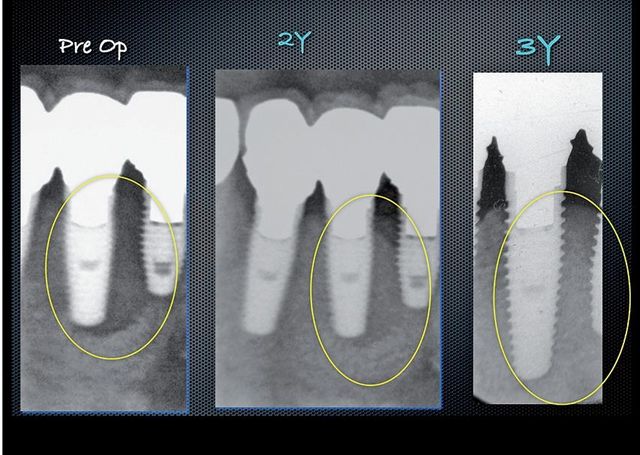
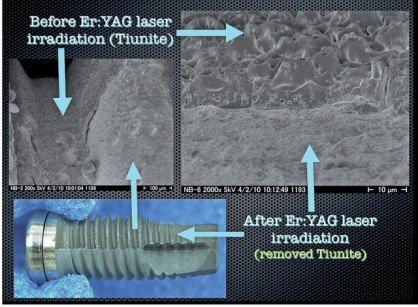
With the rapid advancement of implant dentistry, many complications have been reported in recent years. One of the most serious and frequent of which is peri-implantitis. Numerous articles have discussed risk factors of peri-implantitis as well as ideas to prevent it, however predictable therapy had not yet been developed. Over the years, research has suggested that rough implant surfaces improve the osseointegration of implants. This in turn resulted in implant companies shifting their implant surfaces to have this rougher characteristic. This roughness, however also provided a favorable medium for bacteria once the surface was exposed to the oral environment. When grafting is indicated after bone resorption around an implant, it is extremely difficult to disinfect the surface, thus making the success of the grafting procedure slim. In order to regain the osseointegration, the contaminated surface must be completely removed. The Er:YAG laser is the only equipment to allow this to be accomplished. This reports revolutionary and predictable therapy for peri-implantitis using the Er:YAG laser. The implant surface is irradiated utilizing this laser. Accompanied with water micro-explosions, the Er:YAG laser decontaminates the rough titanium oxide surface of the implant and does so without causing a harmful increase in temperature (Figure 1). Animal research has proved its efficacy to restore osseointegration. In addition, our clinical cases with favorable bone regeneration around the implantbody further reveals evidence of this innovative and predictable peri-implantitis therapy.
Clinical case
The following clinical case illustrates the use of an Er:YAG laser to treat a patient with peri-implantitis: The patient was an 81-year-old female. In September 2006, she received 9 implants in the following tooth sites: numbers 31, and 30 (lower right); 18, 19, 20, 21, and 22, (lower left); and number 11 (upper left). After 4 months, provisional restorations were made and installed. And six months later, final restorations were installed. After 5 years, the patient complained of swelling around the implants. An x ray examination showed considerable resorption around the implants in the region of the first molar.
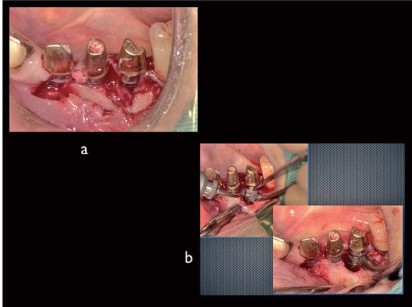
We removed the super-structure and found that the implants was not loose. There are two types of implant periodontal inflammation: perimucositis, where the inflammation is limited to the mucosal membrane; and peri-implantitis, where the inflammation goes all the way to the bone. This is a case of peri-implantitis. And examination determined that this was a CIST (Cumulative Interceptive Supportive Therapy) class D (PD>5mm, BOP+,Bone loss >2mm) case, an we treated periimplantitis with Er:YAG laser irradiation. After giving the patient a local anesthetic (2% xylocaine), the upper portion of the tooth socket was surgically opened and peeled away. Although the implants were not loose, considerable bone resorption and granulated soft tissue (Figure 2a). First the infected granulation tissue was ablated and removed by laser irradiation using a PS600T tip at 50 mJ power and 20 pps, with 5 cc per minute sterilized water spray. Granulation tissue is normally removed with a curette, but bleeding prevents the doctor from having a clear view of the treatment area when using a curette.
In contrast, the Er:YAG laser with water spray eliminates this problem. The application of spray and the micro-explosions caused by the laser light hitting the water keep the treatment area clearly visible. After removing the infected granulation tissue, the contaminated implant surface was sterilized by ablating a layer of TiUnite. A PS600T tip (the flat quartz tip tapers from 600 μm in the upper part to 400 μm in the lower part), was lightly guided over the surface at 50 mJ power and 20 pps with 5 cc per minute water spray. A contaminated layer was stripped away by the microexplosions caused by the Er:YAG laser’s reaction with the water spray. Slightly dark grey areas could be seen on the ablated surface; this was not carbonization but rather the new titanium surface showing through (Figure 2b). As in this case, implants are usually placed more or less vertically, and when the laser is applied perpendicular to the implant, it can easily reach detailed features of the threads and thoroughly sterilize the contaminated titanium oxide layer by stripping way an even layer.